
Amanda van Beinum, Carleton University and Sonny Dhanani, L’Université d’Ottawa/University of Ottawa
How long should doctors wait after a “flatline” appears before they can declare a person dead? How can they be sure that heartbeat and circulation will not return?
The most common way that people die is after their heart stops beating. However, there is limited evidence for how long to wait to determine death once the heart stops. This missing information has repercussions for clinical practice and for organ donation.
A fundamental principle of organ donation is the dead donor rule: donors must be dead prior to recovery of organs, and organ recovery must not be the cause of death. A lack of evidence about how long to wait before declaring death creates a tension: if doctors wait too long after the heart stops, the quality of organs begins to decline.
On the other hand, not waiting long enough introduces the risk of going ahead with organ recovery before death has actually occurred.
Our interdisciplinary team of doctors, bio-engineers and experienced clinical researchers has spent the past decade studying what happens when a person dies after their heart stops. We focused on patients in the intensive care unit who died after life support was withdrawn, since these patients may also be eligible for organ donation.
In particular, we were interested in understanding whether it is possible for the heart to restart on its own, without any interventions like cardiopulmonary resuscitation (CPR) or medication.
A closer look at end-of-life flatline
Our recent study, published in the New England Journal of Medicine, presents observations of the dying process of 631 patients across Canada, the Czech Republic and the Netherlands who died in an intensive care unit. All patients’ families consented to participate in the research.
In addition to collecting medical information about each patient, we built a computer program to capture and review heart rate, blood pressure, blood oxygenation level and respiratory patterns directly from bedside monitors. As a result, we were able to analyze end-of-life flatline patterns for 480 out of 631 patients — including looking at whether and when any circulation or heart activity returned after stopping for at least one minute.
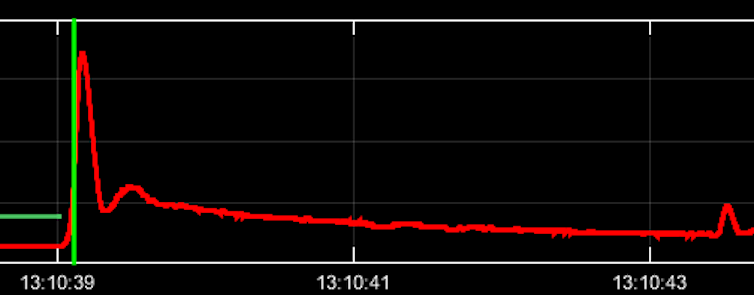
As it turns out, the classic flatline of death is not so straightforward. We found that human heart activity often stops and restarts a number of times during a normal dying process.
Out of 480 “flatline” signals reviewed, we found a stop-and-start pattern in 67 (14 per cent). The longest that the heart stopped before restarting on its own was four minutes and 20 seconds. The longest time that heart activity continued after restarting was 27 minutes, but most restarts lasted just one to two seconds. None of the patients we observed survived or regained consciousness.
We also found it was common for the heart to continue to show electrical activity long after blood flow or pulse stopped. The human heart functions as a result of an electrical stimulation of nerves that causes the heart muscle to contract and contribute to blood flow — the pulse you can feel in your arteries and veins.
We found that the heart rate (electrical stimulation leading to movement of the heart muscle) and pulse (movement of blood in the veins) only stopped together in 19 per cent of patients. In some cases, electrical activity of the heart continued for over 30 minutes without resulting in any circulation of blood.
Why understanding death matters
The results of our study are important for a few reasons.
First, the observation that stops and restarts of heart activity and circulation are often part of the natural process of dying will be reassuring to doctors, nurses and family members at the bedside. Intermittent signals on bedside monitors can sometimes be alarming if observers interpret them as signs that life is unexpectedly returning. Our study provides evidence that stops and starts are to be expected during a normal dying process without CPR, and that they do not lead to regained consciousness or survival.
Second, our finding that the longest pause before heart activity restarted on its own was four minutes and 20 seconds supports the current practice of waiting five minutes after circulation stops before declaring death and proceeding to organ recovery. This helps to reassure organ donation organizations that practices of determination of death are safe and appropriate.
Our results will be used to better inform policy and guidelines for the practice of organ donation internationally. For donation systems to work, when someone is declared dead, there must be trust that the declaration is really true. Trust allows families to choose donation in a time of grief and allows the medical community to ensure safe and consistent end of life care.
This study is also important for improving our broader understanding of the natural history of death. We have shown that figuring out when dead is really dead is perhaps not so simple. It requires careful observation and close physiologic monitoring of the patient. In addition, it requires an understanding that, just as in life, there are many patterns that the dying process can take.
Our work is a step towards appreciating the complexity of dying and suggests we must move beyond the idea of a straightforward flatline to indicate when death has occurred.
This article was co-authored by Laura Hornby, research manager and consultant at the Children’s Hospital of Eastern Ontario Research Institute and Canadian Blood Services, and Nathan Scales, biomedical engineer and research associate at the Dynamical Analysis Lab at the Ottawa Hospital Research Institute.
Amanda van Beinum, PhD Candidate, Sociology, Carleton University and Sonny Dhanani, Associate Professor, Faculty of Medicine, L’Université d’Ottawa/University of Ottawa
This article is republished from The Conversation under a Creative Commons license. Read the original article.

