
Peter Hall, University of Waterloo
Amid the carnage of the First World War, a flu epidemic took hold in the front-line trenches and subsequently spread around the world, infecting one-quarter of the world’s total population and ultimately killing more people than the war itself.
Before it was over, somewhere between 50 million and 100 million people died from what became known as “the Spanish flu.” The currently accepted mortality rate for the Spanish flu is between one and three per cent, and its total mortality numbers are shocking in part because of its widespread reach, proliferating throughout country after country around the globe.
A familiar name
The Spanish flu pandemic was triggered by a virus that is now a household name: H1N1. H1N1 resurfaced in 2009, again spreading to the far reaches of the planet, but with only a small fraction of the death toll of its first emergence.
Although it was not an identical virus, it could have been equally deadly in theory, in part because of its potential to kill people who were younger in age and not otherwise considered vulnerable to flu-related mortality. The absolute mortality rate of the 2009 H1N1 pandemic was 0.001-0.007 per cent. The total number of dead in this case was in the hundreds of thousands around the globe, with a disproportionate number believed to be affected in southeast Asia and Africa.

Why the vast differences in mortality? These two versions of H1N1 did not have the same origin, and there is also an evolutionary push for subsequent versions of the same virus to be less deadly. So the two versions of H1N1 would have been different in these respects.
But, importantly, the world was different too. The conditions under which the Spanish flu overtook the world were abhorrent. The First World War had been raging for several years, and the front lines where the illness emerged were places where young soldiers lived among corpses, rats and contaminated water, and had limited opportunities for personal hygiene.
In 2009, even the most poor nations of the world had better living conditions than those experienced by the average soldier in the trenches of First World War. Despite this, the nations that had the least ability to provide clean environments for their populations were hit the hardest by the H1N1 infections, with large numbers infected and many fatalities.
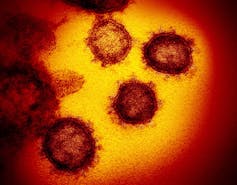
The spread of COVID-19 in China — and recent cases appearing closer to home — has people worried about another Spanish flu scenario. This will not be another Spanish flu, but we have an important opportunity to control the proliferation of the virus within our own populations.
Behaviour and herd immunity
Herd immunity is a concept that comes from the field of zoology. It refers to the ability of a population of animals to resist infection by a pathogen — such as a virus — because a sufficiently large number of individuals within the population have humoural immunity on an individual level. Humoural immunity is the ability of the immune system to form antibodies against a specific infectious agent.
With herd immunity, transmissibility in a population is dramatically reduced via immunological mechanisms. This is the theory behind vaccines, which boost specific immunity within (ideally) a very large proportion of the population, such that a transmissible disease never gains a foothold.
Notice the term “immunological mechanism,” and consider whether the same principle could apply on a behavioural level.
As the body’s humoural immune responses deflect infection, so do behaviours that block routes into the body for an infectious agent. With a very large proportion of the population consistently implementing behaviours that reduce transmissibility, epidemics can be prevented or vastly limited, without the reactionary measure of quarantine.
Just as humoural immunity does not convey perfect protection to the individual, the same is true for behavioural immunity; it is simply important that a very high proportion of the population is performing precautionary behaviours consistently. Protection is on the level of the herd, more so than on the level of the individual.
Are we talking about the wrong things?
In the context of this concept of “behavioural herd immunity,” current discussions about COVID-19 in conventional and social media may be focused on the wrong things. Rather than talking about fear-inducing counterfactual scenarios (what ifs), we need to focus on crowdsourcing strategies that limit the ability of the infection to get a foothold in our population.
Read more: Coronavirus fears: Should we take a deep breath?
A vaccine would be nice and will eventually arrive. But in the meantime, epidemics like COVID-19 can be prevented by increasing the prevalence of precautionary behaviours in the general population that impede its spread.
These measures include a few familiar maxims, none of which are implemented consistently enough, and a few unfamiliar ones, which very much need to be taken up individually en masse. And soon.
The familiar ones:
- wash your hands frequently and properly;
- cover your mouth (with your arm) when coughing or sneezing;
- avoid close contact with those who are already infected.
Before brushing off the above as obvious, we should ask ourselves: do we do these with complete consistency? Can we do better? Consider also the following less obvious but equally important behaviours:

1. Disinfect your mobile device screen twice per day — it is a portable petri dish, accumulating bacteria and, yes, viruses. Antibacterial wipes are necessary here, as they generally kill viruses as well. Clean your device at least twice daily, once at lunch and once at dinner time (or linked to another daily routine). A recently published study estimates that viruses like COVID-19 may be able to persist for up to nine days on smooth glass and plastic surfaces, like a mobile phone screen.
2. Avoid touching your face. Your mouth, nose, eyes and ears are all routes into your body for viruses, and your fingers are constantly in touch with surfaces that may contain viruses. This simple measure is very hard to maintain consistently, but is essential for infection control.
3. Use masks only if you are yourself ill and give social kudos to people who are responsible enough to use them when sick.
4. Self-quarantine if you are ill and have a fever.
5. Engage your social network to brainstorm other simple behavioural changes.
Preventing spread
Strengthening herd immunity through behaviour is critical to preventing COVID-19 spread. We need to be talking about it more, and doing it more. In the sea of fear-provoking uncertainties, this is something that we are in control of individually and en masse.
Let’s do better about implementing the above precautionary behaviours with high consistency, and over the long-term.
And here’s a side benefit: we will be preventing many other infectious illnesses from spreading, including seasonal influenza, which kills more people in an average month than COVID-19 did last month.
Peter Hall, Professor, School of Public Health and Health Systems, University of Waterloo
This article is republished from The Conversation under a Creative Commons license. Read the original article.

