
Alister McNeish, University of Reading
With the recent outbreak of the COVID-19 virus have come reports that people taking drugs called ACE inhibitors to treat high blood pressure might be at higher risk of death. This has led many to ask what are ACE inhibitors and what do they do?
What are ACE inhibitor drugs?
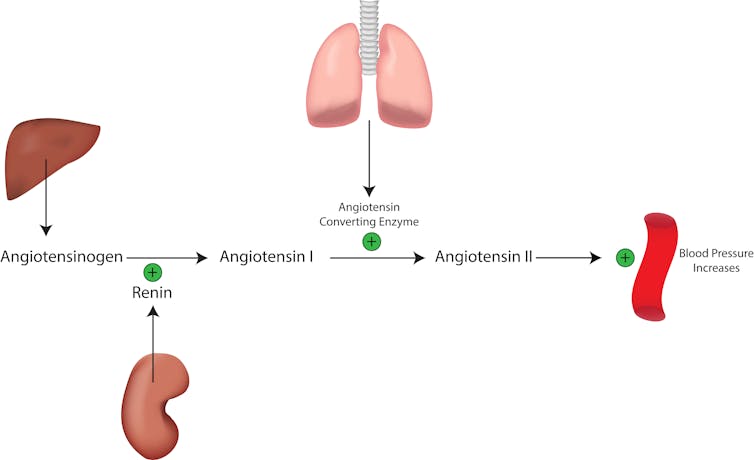
Angiotensin converting enzyme (ACE) inhibitors are commonly used to treat hypertension (high blood pressure) and several other cardiovascular diseases. ACE inhibitors are widely used due to their effectiveness and safety and many types exist – generic names for these drugs all end in “pril”. They target an enzyme called angiotensin-converting enzyme (ACE) which is found in certain cells of the lungs and those that line blood vessels throughout the body. ACE’s normal function is part of the renin–angiotensin–aldosterone system, which helps to regulate blood pressure as well as water balance and sodium, an electrolyte that is vital for balancing the water in and around your cells, muscle and nerve function and stable blood pressure.
How do these drugs work?
When the kidneys sense low sodium or drops in blood pressure they release an enzyme called renin into the bloodstream. Renin starts a cascade of events leading to the production of angiotensin II, a hormone that increases the retention of sodium in the kidney helping the body to conserve water and sodium. In addition, angiotensin II increases the constriction of blood vessels which in turn increases blood pressure.
Angiotensin II is produced by the conversion of a protein called angiotensin I, which circulates in the blood, by both ACE and ACE2 enzymes. Therefore, targeting ACE with ACE inhibitors leads to reduced levels of angiontensin II, meaning that blood vessels will be less constricted and less sodium and water will be retained by the kidneys which lowers your blood pressure.
The reason ACE inhibitors are so effective at lowering blood pressure is that many people with hypertension have an overactive renin–angiotensin–aldosterone system and so angiotensin II levels in the blood can be high. Therefore, this type of drug is often used as a first line of treatment or in combination with other drugs that lower blood pressure.
Read more: What is a healthy blood pressure?
Why are drugs that lower blood pressure being associated with the respiratory syndrome associated with COVID-19?
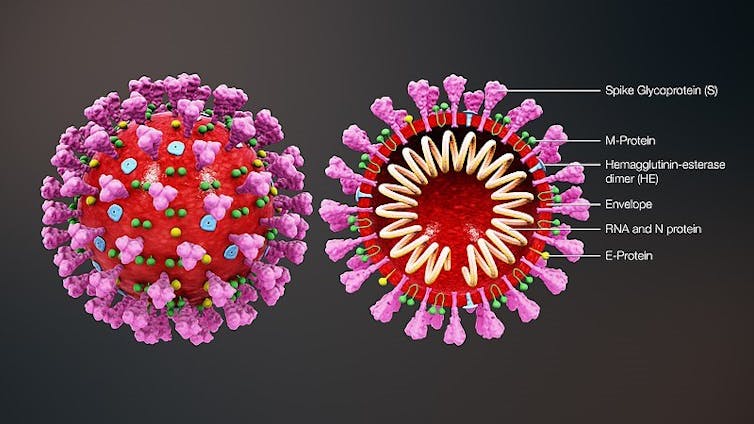
It’s largely down to that target of ACE inhibitors – however it’s the related ACE2 that seems to be the target that the virus uses to enter the body. As ACE2 has a high density in the endothelial cells (which line all blood vessels) in the lungs a link seems obvious but does not explain why ACE inhibitors are being linked to increased mortality.
The link seems to be two-fold. Data from those who have died from COVID-19 in China show that almost 50% had high blood pressure, diabetes or other disease associated with treatment with ACE inhibitors. Evidence in patients without COVID-19 infection suggests that ACE inhibitors (and their close relatives ARBs, aka “sartans”) can lead to increased expression of ACE2, an effect apparently not seen with other drugs used to treat hypertension. Combining the evidence leads to the suggestion ACE inhibitors increase the binding target of COVID-19 infection.
Should I be worried?
Despite the attention, there is no direct evidence that it is ACE inhibitors that cause increased mortality. First – age seems to be the primary risk factor for COVID-19 mortality and rates of high blood pressure in the elderly are high, estimated to be over 60% in the over 60s. No assessment of treatment for hypertension in mortality was undertaken in the Chinese studies meaning hypertension rates simply reflect patient demographics. Second, many patients with high blood pressure already have an overactive renin–angiotensin–aldosterone system which could mean an increased ACE2 expression regardless of treatment.
Therefore, with no direct evidence that ACE inhibitors cause increased mortality in COVID-19 infection the best current advice is to continue taking these medications as directed.![]()
Alister McNeish, Associate Professor in Cardiovascular Pharmacology, University of Reading
This article is republished from The Conversation under a Creative Commons license. Read the original article.

