Former Atlanta Police Officer Matthew Johns was sentenced this evening to 20 years to serve 5.

USA & CANADA (901)
Latest News
Donald Trump is taking hydroxychloroquine to ward off COVID-19. Is that wise?
Wednesday, 27 May 2020 00:13 Written by theconversationThe White House’s confirmation that US President Donald Trump has been taking hydroxychloroquine every day for the past two weeks, with his doctor’s blessing, has reignited the controversy over the drug. It has long been used against malaria but has not been approved for COVID-19.
Trump said he has “heard a lot of good stories” about hydroxychloroquine, and incorrectly claimed there is no evidence of harmful side-effects from taking it. His previous claims in March that the drug could be a “game changer” in the pandemic prompted many people, including Australian businessman and politician Clive Palmer, to suggest stockpiling and distribution of the drug to the public.
But the dangers of acting on false or incomplete health information were underlined by the death of an Arizona man in March after inappropriate consumption of the related drug chloroquine. It’s important to know the real science behind the touted health benefits.
How do these medicines work?
Hydroxychloroquine is an analogue of chloroquine, meaning both compounds have similar chemical structures and a similar mode of action against malaria. Both medications are administered orally and have common side-effects such as nausea, diarrhoea and muscle weakness. However, hydroxychloroquine is less toxic, probably because it is easier for the body to metabolise.
Chloroquine and hydroxychloroquine are listed by the World Health Organisation as an essential medicine. Both drugs have been used to treat malaria for more than 70 years, and hydroxychloroquine has also proved effective against auto-immune diseases such as systemic lupus erythematosus and rheumatoid arthritis. The US Food and Drug Administration has approved both chloroquine and hydroxychloroquine for treating malaria, but not for COVID-19.
Read more: In the rush to innovate for COVID-19 drugs, sound science is still essential
We don’t know exactly how these drugs work to combat the malaria parasite. But we know chloroquine disrupts the parasite’s digestive enzymes by altering the pH inside the parasite cell, presumably effectively starving it to death.
Malaria parasites and coronaviruses are very different organisms. So how can the same drugs work against both? In lab studies, chloroquine hinders replication of the SARS coronavirus, apparently by changing the pH inside particular parts of human cells where the virus replicates.
This offers a glimmer of hope that these pH changes inside cells could hold the key to thwarting such different types of pathogens.
Is it OK to repurpose drugs like this?
Existing drugs can be extremely valuable in an emergency like a pandemic, because we already know the maximum dose and any potential toxic side-effects. This gives us a useful basis on which to consider using them for a new purpose. Chloroquine is also cheap to manufacture, and has already been widely used in humans.
But we shouldn’t be complacent. There are significant gaps in our understanding of the biology of SARS-CoV-2, which causes COVID-19, because it is a brand new virus. There is a 20% genetic difference between SARS-CoV-2 and the previous SARS coronavirus, meaning we should not assume a drug shown to act against SARS will automatically work for SARS-CoV-2.

Even in its primary use against malaria, long-term chloroquine exposure can lead to increased risks such as vision impairment and cardiac arrest. Hydroxychloroquine offers a safer treatment plan with reduced tablet dosages and lessened side-effects. But considering their potentially lethal cardiovascular side-effects, these drugs are especially detrimental to those who are overweight or have pre-existing heart conditions. Despite the urgent need to confront COVID-19, we need to tread carefully when using existing medicines in new ways.
Any medication that has not been thoroughly tested for the disease in question can have seriously toxic side-effects. What’s more, different diseases may require different doses of the same drug. So we would need to ensure any dose that can protect against SARS-CoV-2 would actually be safe to take.
The evidence so far
Although many clinical trials are under way, there is still not enough evidence chloroquine and hydroxychloroquine will be useful against COVID-19. The few trials completed and published so far, despite claiming positive outcomes, have been either small and poorly controlled or lacking in detail.
A recent hydroxychloroquine trial in China showed no significant benefits for COVID-19 patients’ recovery rate. A French hydroxychloroquine trial was similarly discouraging, with eight patients prematurely discontinuing the treatment after heart complications.
The fascination with chloroquine and hydroxychloroquine has also adversely affected other drug trials. Clinical trials of other possible COVID-19 treatments, including HIV drugs and antidepressants, have seen reduced enrolments. Needless to say, in a pandemic we should not be putting all our eggs in one basket.
Then there is the issue of chloroquine hoarding, which not only encourages dangerous self-medication, but also puts malaria patients at greater risk. With malaria transmission season looming in some countries, the anticipated shortage of chloroquine and hydroxychloroquine will severely impact current malaria control efforts.
Read more: Coronavirus: scientists promoting chloroquine and remdesivir are acting like sports rivals
Overall, despite their tantalising promise as antiviral drugs, there isn’t enough evidence chloroquine and hydroxychloroquine are safe and suitable to use against COVID-19. The current preliminary data need to be backed up by multiple properly designed clinical trials that monitor patients for prolonged periods.
During a pandemic there is immense pressure to find drugs that will work. But despite Trump’s desperation for a miracle cure, the risks of undue haste are severe.
This article was coauthored by Liana Theodoridis, an Honours student in Microbiology at La Trobe University.
Teresa G. Carvalho, Senior Lecturer in Microbiology, La Trobe University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Nancy Pelosi Fat-Shames Donald Trump, Says He's Morbidly Obese, He Replies Her Saying She Has Mental Problem
Sunday, 24 May 2020 23:06 Written by toriHow coronavirus is contributing to drug shortages in Canada
Thursday, 14 May 2020 04:34 Written by theconversation 
Lorian Hardcastle, University of Calgary and Reed F Beall, University of Calgary
COVID-19 has exposed and magnified weaknesses within health-care systems. Drug shortages, which are a growing problem in Canada, may be one example of this.
Shortages hinder patients’ ability to effectively manage chronic diseases, leading to unnecessary harm. They also complicate the work of health-care providers, such as pharmacists, who must spend considerable time trying to find difficult-to-obtain drugs, and physicians, who have to prescribe alternative drugs to replace those that are unavailable. Shortages may also increase costs if alternative treatments are more expensive.
Potential contributors to shortages
Disruptions in the supply chain due to COVID-19 may cause shortages because many drugs and the raw ingredients used to produce them come from India and China. India has started to ban some drug exports due to shortages in its own country.
Supply-side pressures are also caused by increasing consolidation in the pharmaceutical industry, which means fewer suppliers and manufacturing facilities and thus fewer alternative sources for drugs. Given that most shortages are of less expensive generic drugs, some speculate that manufacturers intentionally limit the production of less profitable products to drive up sales of expensive brand name drugs.
COVID-19 may also produce demand-side shortages. Manufacturers are struggling to keep up with demand for the sedatives required by patients on ventilators. Large volumes of these drugs will also be necessary when Canadian hospitals catch-up on elective surgeries cancelled due to COVID-19. For example, two manufacturers of one such sedative, propofol, have reported recent shortages.

Hydroxychloroquine and azithromycin, which were touted as treatments for COVID-19, are in sufficiently high demand that professional regulatory bodies have issued warnings about inappropriately prescribing these products. Since March 15, six azithromycin products and one hydroxychloroquine manufacturer have reported shortages in Canada. The latter of these affects patients who take hydroxychloroquine to treat arthritis and lupus.
Prevalence of shortages
In order to enhance tracking of and responsiveness to drug shortages, Health Canada has required manufacturers to report shortages since 2017. Shortages have been steadily increasing over the past two years, with 2,023 products in shortage as of April 2020.
Some of this effect may be attributable to the increasing number of products that are added to the pharmaceutical market each year. This suggests that Health Canada must continue to increase its capacity to monitor and address shortages to correspond with the growing number of products in active use. In its role as federal drug regulator, Health Canada may help drug manufacturers address shortages by reviewing alternative suppliers, processes, facilities and production locations.
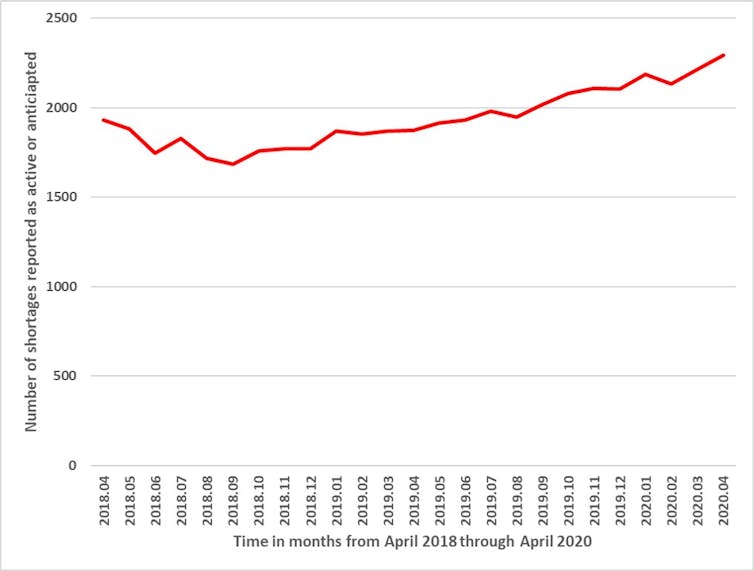
Although the full effects of COVID-19 on drug shortages are not yet known, it is notable that manufacturers reported 221 new shortages in April 2020, compared to 148 in March, 59 in February and 104 in January. In other words, a recent increase in shortages, which could be attributable to COVID-19, may worsen existing problems with shortages.
Response to shortages
Pharmacists reported a rush to fill prescriptions when physical distancing measures took effect, with some patients requesting a six-month supply. In response, Health Canada discouraged drug stockpiling and the Canadian Pharmacists Association and provincial governments strongly encouraged pharmacists to limit patients to a 30-day supply of their prescriptions.
Although this may help to address shortages by moderating demand, it increases the cost of drugs for individuals who may incur additional dispensing fees with each visit. This disproportionately affects those who are unemployed and who have lower incomes. It may also require more frequent visits to pharmacies, which can be dangerous for seniors who are at increased risk for COVID-19 and tend to use more prescriptions. When this 30-day restriction is lifted, the elevated demand may further contribute to shortages.
The federal government has implemented several measures to address COVID-related shortages. On March 25, it authorized the passage of regulations necessary for “preventing shortages … or alleviating those shortages or their effects, in order to protect human health.”
This legislation also allows the government to grant a manufacturer a license to produce a drug, even if another manufacturer holds the patent for that product. Although these licences could theoretically increase supply, practical challenges may limit their utility. For example, alternative suppliers may similarly be unable to obtain raw ingredients from the same foreign suppliers.
A more practicable solution may be the import and sale of drugs that have not yet met all Canadian regulatory requirements, which is permissible following an order by the minister of health. However, this exceptional process is only available for particular drugs that meet certain manufacturing standards.
While the federal government’s efforts may help to mitigate shortages during COVID-19, it should also seize this opportunity to develop long-term solutions to shortages, which have affected the Canadian drug market for years. Due to the globalization of pharmaceutical manufacturing, the government must work with both industry and other countries to rapidly identify and respond to disruptions in the supply chain, so that Canadians have uninterrupted and reliable access to safe drugs. Given the pressures caused by COVID-19, now is a pivotal time for the government to act.![]()
Lorian Hardcastle, Assistant Professor, Faculty of Law and Cumming School of Medicine; Member, AMR One Health Consortium, University of Calgary and Reed F Beall, Assistant Professor, Community Health Sciences, Cumming School of Medicine, University of Calgary
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Man, 41, arrested for posing as Canadian Army Officer
Wednesday, 06 May 2020 20:17 Written by myjoyonlineThe Ghana Military Police has arrested 41-year-old Bernard Ayeh of Adjiringanor, a suburb of Accra, for allegedly personating as a Canadian Army Officer.
The said suspect was picked up around the Adentan Barrier general area wearing a camouflage uniform while driving a Mazda saloon car with registration number GR1406-20, a statement signed by Colonel E. Aggrey-Quashie, the Director of Public Relations, Ghana Armed Forces, said.
Bernard Ayeh, the statement said, had in his possession two different types of pistols (a Walther PPS Pistol Serial Numbered AK5810 with 15 rounds and a Springfield Armory XD-9 Pistol Serial Numbered XD883001).
He also had two pistol holsters, two handcuffs with keys, a jack knife, a baton, two fake Canadian Army Identity Cards, bearing the name Lieutenant Colonel Bernard Ayeh, three mobile phones and an amount of ¢13,470.40.
Bernard Ayeh, the statement said, was earlier spotted by a Senior Officer of the Ghana Army around Peduase, but he sped off upon sighting the Ghana Army vehicle and thereby raising suspicion.
The Military Police was notified while the Senior Officer and his aides pursued him to the Adentan Barrier where he was eventually nabbed.
Upon interrogation, the statement said, he confessed that he was not a Canadian Army Officer and that he once worked as a contractor with the Canadian Army, during which he acquired the Canadian Army camouflage uniform.
He also disclosed that he bought one of the pistols from an official at the Ghana Police Headquarters, while he inherited the other one from a late Uncle.
Further checks by the Military Police also revealed the suspect’s name had come up in an investigation in respect of personating a military officer and other matters under investigation before the investigative agencies.
The Military Police had, accordingly, processed the suspect for referral to the Police Headquarters for further investigation and possible prosecution.
It, therefore, urged any member of the public who had fallen victim to the activities of the suspect to go forward to assist in investigations.
Popular News
5-year-old boy is pulled over by Police while driving his parents' SUV to California to buy a Lamborghini with $3 (Video)
Wednesday, 06 May 2020 00:56 Written by lindaikejiblogA 5-year-old boy left a police officer shocked after he found him driving his parents' car during a traffic stop.
Trooper Rick Morgan noticed a driver inside an SUV driving erratically and switching between lanes on a freeway in Ogden, Utah just before noon on Monday. When he pulled the car over, Morgan said he was shocked to find a young boy behind the wheel.
'My speedometer showed 32 miles-per-hour,' Morgan told Fox 13. 'It amazed me that when he heard my siren, he did pull over and stop.'
'When I got to the window and the window came down, I wasn't quite sure what to think. It was pretty clear when the window came down, it was a young, very underage driver.'
When asked where he had been driving to, the boy replied 'California.'
The 5-year-old reportedly told troopers that he left the house following an argument with his mother after she told him she wouldn't buy him a Lamborghini.
Police say he had been trying to reach his sister's house in California and had planned to buy a Lamborghini when he got there, with the three dollars in his purse.
'It likely would have been much worse had he gone much further,' Morgan told the publication. 'He was sitting on the front edge of his seat so he could reach the brake pedal.'
The boy has since been reunited with his parents.
Watch the video below.
Coronavirus bailouts won’t save startup workers from layoffs
Tuesday, 05 May 2020 00:53 Written by theconversation 
As financial markets tumble, investors are pulling funding from startups. Sales for anything but bare essentials have evaporated, while progress on product development and market testing has halted for work that requires in-person collaboration.
Many existing bailout plans are targeted for larger enterprises in industries like aviation and tourism. While limited resources are explicitly earmarked for startups and other small enterprises, they come with stringent criteria and complex and slow application processes.
Many startups already function without cash reserves and lines of credits. Unlike larger resource-rich companies, startups are unable to make pledges to avoid layoffs. This confluence of events means that startups and the jobs within them are vanishing and at a pace that likely exceeds job dissolution in larger, more established firms.
An abrupt ending
The CEO of a startup I’ve been studying for more than two years was forced to cut costs by 50 per cent at the request of a cash-strapped investor. He accomplished this by slashing his own salary to nothing, eliminating positions in the management and sales teams, closing a physical office and severing outsourcing arrangements.
Days later, his major investor said these cuts were inadequate. The CEO explored alternatives, including cutting back to a skeletal staff and seeking government funding to help get through this time. His company fell through the cracks of any bailout schemes. Cutting back staff would halt any progress in product development and the ability to complete desperately needed sales.

He shuttered the company 10 days after making his first round of cuts, leaving more than 30 employees without jobs. He’s working with investors to offer former employees up to a month’s severance. He and another member of the management team are on WhatsApp and email offering support to former employees as they work through the end of the organization and formulate plans to help them enter an extremely challenging labour market.
For months before the coronavirus hit, many of the employees were already concerned about whether the company would ever find the right market fit. Yet, the investors remained prepared to keep investing to bring a fully developed product to market until the pandemic.
Hastening the demise
Versions of this story are unfolding in startups and small enterprises globally. Some are limping by with pay cuts, furloughs, layoffs and other cost-cutting measures. For many others, the coronavirus has brought about their demise.
The specific circumstances vary. Acquisitions fall through. Startups fail to find product market fit. Their technologies never reach their full potential.
Funding for some startups may have been drying up already. Other startups may have been on the road to closure for some time with the coronavirus simply accelerating the inevitable. We’ll never know if the startups that failed might have made it through in other circumstances.
Working for startups is a risky proposition for employees in the best of times. Over the past four years, my team and I have conducted more than 200 interviews with people seeking jobs and working in startups and those doing the hiring.
The tradeoffs of working for startups
Most of them recognize the tradeoffs inherent to working for a startup. They accept lower levels of stability, salary, career opportunities and resources in exchange for being able to have a larger effect on the direction of the business and greater flexibility in their roles.

When asked what they would do if their organization failed, many said that they would seek a similar role in another startup.
This risk-taking made sense in a thriving ecosystem where startups were scrambling to find talent and a new job was often just days away. Yet it’s not clear how well startup experience transfers to more established companies. In tight labour markets, it may be valued. When millions are newly unemployed, it is less clear what the prospects of former startup employees will be.
Not the same for everyone
This is just one of the many ways that the effects of the coronavirus are unequal. The disease itself has not hit jurisdictions, countries, continents or demographic groups at an even pace. The economic costs of coping with the disease are not equal for already impoverished communities and those with deeper resources.
Jobs are also vanishing for those working in brick-and-mortar retail and restaurants, and for many gig workers who were rarely in the best paying, most secure jobs to begin with. Nor are the lingering after-effects of this crisis likely to be felt in the same way by all.

Still some are predicting a renaissance boom following this pandemic with a wave of innovations leading to the founding of new startups.
Read more: The coronavirus crisis: A catalyst for entrepreneurship
After all, the original Renaissance followed the Black Death. Crises of many varieties may plant the seeds of innovation.
But little is known about what a new renaissance would look like — and who will reap its benefits.
Lisa Cohen, Associate Professor, Business Administration, McGill University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Why religious freedom stokes coronavirus protests in the U.S., but not Canada
Tuesday, 05 May 2020 00:43 Written by theconversation 
Pamela E. Klassen, University of Toronto
Religious freedom, cherished as an American ideal, has been frequently invoked in the United States during protests against COVID-19 public health measures.
In Canada, forms of protests — including by churches — are more likely to focus on the systemic underfunding of long-term care and homeless shelters or the lack of sufficient medical and water infrastructure in Indigenous communities.
Why the difference?
Across the U.S., conservative Christians flouted state and municipal social distancing orders as late as March 31, sometimes by overtly breaking the law, claiming that God, not the state, will protect the people.
During the Christian Holy Week, evangelical and Pentecostal church leaders, often backed by Republican politicians, brought lawsuits against state and municipal governments, arguing that curtailing religious gatherings for the sake of limiting the spread of COVID-19 was a breach of religious freedom.

With lightning speed, federal and state lawyers weighed in on the balance between public health measures and religious liberty.
By contrast, the story in Canada is largely one of religious organizations of all varieties co-operating with public health measures. To date, there is no equivalent in Canada of these high-profile COVID-19 legal battles in which churches reject both public health directives and state legislation.
Suspicion of science, government
Religiously based suspicion of scientific and government authority is not unique to conservative Christians; Hasidic Jewish communities share these suspicions and constitute a significant number of those infected with COVID-19 in New York state.
Even in the case of Hasidic Jews, however, the border might make a difference: Hasidic communities in Québec have been praised for their diligence in adhering to social distancing, in contrast to those in New York, where some rabbis have mocked public health recommendations.
The contrasting responses to COVID-19 in Canada and the United States are rooted in very different national attitudes about individual and collective responsibility for public health.
In the United States, Democratic front-runner Joe Biden may come to embrace Bernie Sander’s plan for “Medicare for All,” but even the devastating reality of being the country hardest hit so far by COVID-19 has not seemed to turn the tide of public opinion on the need for universal medicare.
In Canada, by contrast, leaders across the political spectrum are throwing their support behind public health care, with even some conservative politicians calling for more funding, especially for long-term care. While Donald Trump tweeted a call to anti-public health protesters to “liberate” their states, in Ontario, Conservative Premier Doug Ford dismissed a scattering of such protesters in Toronto as selfish “yahoos.”
Invoking religious freedom in an attempt to opt out of health-care legislation is much more common in the U.S. than Canada. Both countries protect religious freedom, dating back to 1791 in the United States with the First Amendment of the constitution guaranteeing the “free exercise” of religion, while in Canada, the Canadian Charter of Rights and Freedoms has protected the “freedom of conscience and religion” since 1982.
Religious freedom as a rallying cry
These parallel guarantees, however, stem from very different histories of using religious freedom as a rallying cry, including to resist public health care. I’ve discussed this in my research, especially in relation to women’s reproductive health.
In the wake of former U.S. president Barack Obama’s Affordable Care Act, for example, Catholics and evangelical groups used a religious freedom argument to contest the new mandate that their health insurance plans provide access to contraception for women employees.

In Canada, the less frequent citing of religious freedom rights in the courts to curtail health-care access may be related to a wider acceptance of health care as a public good and a basic human right.
In both Canada and the U.S., the struggle for publicly funded health care in the mid-20th century depended on coalitions of politicians, medical professionals and religious leaders. In Canada, a Baptist minister-turned-politician, Tommy Douglas, galvanized the country with a vision that public health care for all was a human right and, for some, also a religious obligation.

Similarly, in the U.S., when Dr. Montague Cobb, leader of the National Medical Association, successfully argued for Medicare before Congress in 1965, he concluded his testimony with a Christian hymn.
The Canadian version of public health care, however, now serves a much wider range of the population than Medicare does in the U.S., and has become a cornerstone of Canada’s national identity, with minimal overt connections to religion.
But in the United States, public health care remains a source of profound national and religious division. The current Republican administration regularly uses religious freedom legislation, including conscientious objection rules for health-care providers, to chip away at Medicare, limiting access to health care for women, LGBTQ, poor and rural people.
A time of reckoning is coming when public health measures and public and private health-care delivery will be assessed for their effectiveness during the COVID-19 pandemic. The role of religious communities and the ideals of religious freedom in supporting or impeding public health must be included in this reckoning, especially in the United States.
Pamela E. Klassen, Professor of the Study of Religion, University of Toronto
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Atlanta cop who beat 15-year-old black boy till he went unconscious gets 20-year sentence
Monday, 04 May 2020 02:19 Written by face2faceafricaThe non-white community has been alarmed about police brutalities against African-Americans with some recorded deaths.
Even more harrowing is seeing such rogue cops get away with zero or little punishment as if Black lives don’t matter.
But it has been good news for the African-American community when police officer, Matthew Johns was handed a 20-year sentence this week after he was indicted on eight felonies for beating 15-year-old Antraveious Payne in 2018.
Antraveious Payne’s mother said her son’s behavior changed for the worse and he started to experience chronic headaches after Johns attacked him.
Johns was indicted on eight felonies, including four counts of aggravated assault, two counts of violation of oath by an officer and two counts of giving false statement for repeatedly kicking and choking a 15-year-old boy until he was unconscious and then lying about it.
Johns pleaded guilty on July 10, and was sentenced on Monday to 20 years with five to serve in prison in connection with the 2016 incident reports TFTP.
Disturbing dashcam footage revealed Johns beating the Atlanta teenager even when he offered no resistance, but what made the police officer’s case even bizarre is that Matthew had road crash with his cruiser a few weeks prior and was barred from driving, but managed to check out a vehicle and used it to ram another car, then beat the teen and lied about the entire ordeal.
Matthew Johns was part of the department’s elite Apex Unit doubling as a Marine and on September 15, 2016, in southwest Atlanta, WSB-TV reported then that Antraveious Payne and two teenage suspects riding in a stolen car were given a chase by Zone 3 officers and Georgia State Patrol.
It was during the chase that Johns alighted from his cruiser and kicked Payne in the head. The video also showed he kicked the teen more than once, struck him on his side repeatedly and then was seen kneeling on his neck before punching him in the head while cuffing him.
Johns told investigators he thought the teen was reaching for a gun. But one of his supervisors didn’t think his story added up, especially when the other officers on scene said the three suspects never resisted.
Prosecutors, using the video of the incident, agreed, noting that Payne got out of the car and laid on the ground with his hands up, showing he did not have a weapon and was willing to surrender.
Nevertheless, Johns still beat the hell out of him until the teen fell unconscious. Payne was beaten so badly by Johns that he was hospitalized with a concussion and suffered multiple lacerations to his face.
According to the report, after the incident, Johns was placed on administrative leave and no action was taken until a new police chief took office and reopened the case.
Johns was then fired. However, for beating a compliant suspect for no reason, he faced no criminal charges—until more than a year later.
A lawsuit by Payne or his family is likely to emerge which could cost the taxpayers of Atlanta despite Payne breaching the law by riding in a stolen vehicle because of Johns’ excessive use of force.
It does appear Johns actions are not unique as a recent investigation from the Atlanta Journal-Constitution analyzed 184 fatal police shootings in the state of Georgia since 2010 and according to the data, at least 70 people were shot in the back by police officers.








